— And What Finally Helped Me Manage It

Disclaimer: This article is for informational purposes only and is not a substitute for professional medical advice. Always consult a qualified healthcare provider before making changes to your diet, supplements, or medications.
For a long time, I assumed digestive issues were something you could simply “push through.”
Eat carefully. Get back on routine. Power on.
That approach worked—until it didn’t.
Somewhere after 40, my gut stopped bouncing back the way it used to. Minor disruptions turned into lingering discomfort, which turned into bloating and weight gain. I have to add here that I wasn’t very selective about what I ate. I told myself I was a “foodie,” but it was just an excuse to park a chair in front of my fridge and eat everything inside! (Not literally, but you get the idea.) Stress showed up physically, and situations I once handled without thinking suddenly required more intention.
I didn’t fully understand how much had changed until a flare-up forced me to slow down and pay attention.
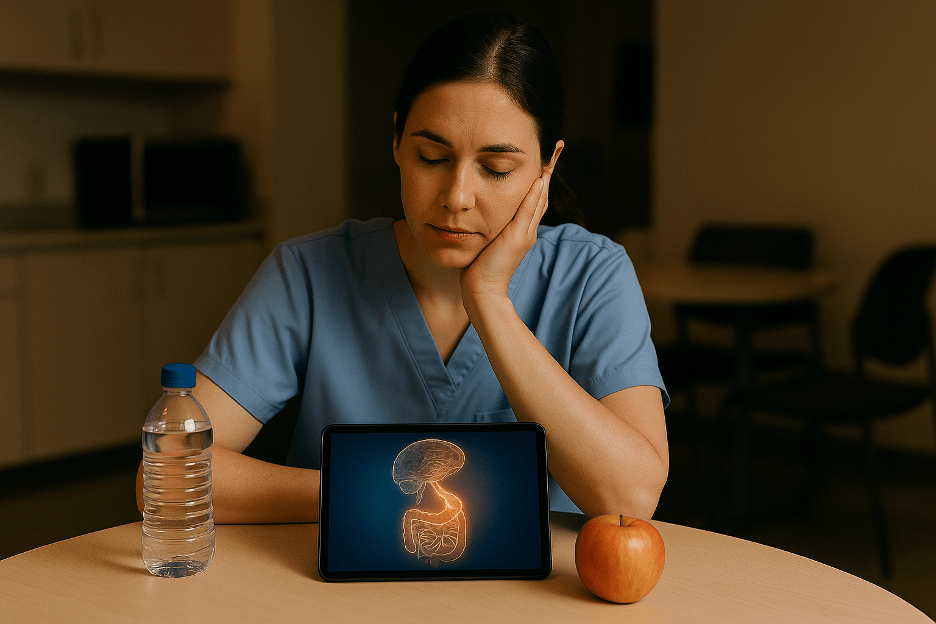
The Moment I Stopped Assuming My Gut Would “Sort Itself Out”
I spent most of my life eating without abandon, never paying attention to what I was shoving into my mouth. Then, while traveling abroad, I experienced a sudden and severe digestive flare-up. It wasn’t dramatic—but it was undeniable.
Navigating an unfamiliar healthcare system while unwell is humbling. Fortunately, I received excellent care and recovered quickly. The diagnosis—gastritis along with H. pylori—came as a surprise, but it also brought clarity.
Thirty days of antibiotics later, I was physically better. But mentally, something had definitely shifted.
Not because something had “gone wrong,” but because I realized something important: My body wasn’t fragile—but it was no longer forgiving of guesswork or bad eating habits.
My experience was a little frightening, but it was even more instructive. It made me rethink how I approached food, stress, and routine—especially during times of change.
Why Gut Health Can Feel More Unpredictable After 40
Later, as I started learning more, it became clear that my experience wasn’t unusual.
As we age, the digestive system doesn’t necessarily fail—but it does become more sensitive to disruption. Stress, illness, sleep changes, and dietary shifts can have a bigger impact than they once did.
As gastroenterologist Dr. Emeran Mayer, author of The Mind-Gut Connection, explains:
“As we age, the gut microbiome becomes less resilient to stressors such as diet changes, illness, and psychological stress, which can make digestive symptoms more noticeable and longer-lasting.”
This framing was reassuring. It wasn’t about doing something wrong. It was about understanding that the margin for error had changed.
Advice that once worked casually —“just eat clean,” “drink more water,” “relax”—is often no longer specific enough. The issue isn’t effort. It’s feedback.
What Actually Helped (When Advice Wasn’t the Problem)
Once I recovered, I didn’t overhaul my life or follow an extreme protocol. What helped was something far less dramatic—and far more sustainable.
I shifted my focus from control to consistency and awareness.
A few things made the biggest difference:
- Keeping familiar, gut-friendly foods available during routine changes
- Staying intentionally hydrated, especially during stressful or busy days
- Paying attention to how stress showed up physically—not just mentally
- Reducing decision fatigue by planning lightly instead of reacting
What surprised me most was this realization:
I didn’t need more advice. I needed a way to notice patterns without obsessing.
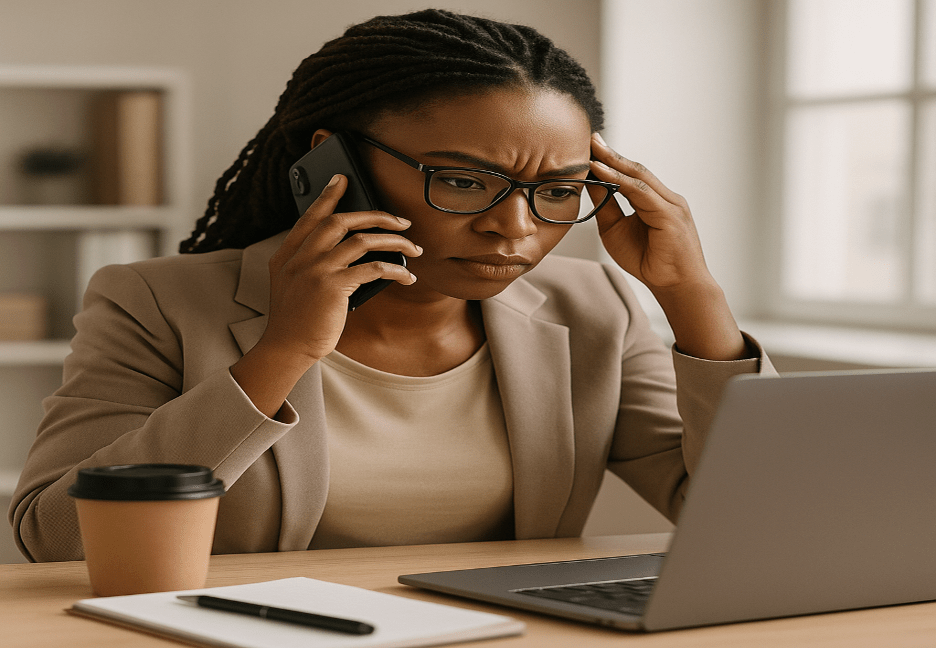
The Role Stress Plays (Whether We Acknowledge It or Not)
Stress and digestion are deeply connected, even when we don’t consciously feel “stressed.”
The gut and brain communicate constantly. When routines shift—such as travel, deadlines, or disrupted sleep—the nervous system often reacts before the mind catches up.
As a neuroscientist and gut researcher, Dr. Michael Gershon notes:
“The gut and brain are in constant communication. Stress doesn’t just affect how we feel emotionally—it can directly influence digestion, motility, and gut sensitivity.”
Simple practices can help more than expected:
- Short breathing exercises
- Gentle stretching or walking
- Brief moments of pause before meals
Not to “fix” anything—but to reduce background noise.
The gut responds to the environment as much as food. Recognizing that changed how I approached daily life.
Why Tracking Became More Helpful Than Guessing
Over time, it became clear that the hardest part wasn’t knowing what to do—it was remembering, noticing, and adjusting without overthinking.
I needed a way to:
- See which patterns are repeated
- Understand what helped during disruptions
- Reduce mental load instead of adding to it
“That’s where simple tracking becomes useful—not as control, but as support.”
Gastroenterologist Dr. Will Bulsiewicz, author of Fiber Fueled, puts it this way:
“Understanding patterns in symptoms is often more helpful than focusing on individual foods or isolated behaviors.”
When you can see patterns, you stop blaming yourself for symptoms that actually have context.
A Note on Tools (Not Fixes)
If you’re navigating gut changes after 40, tools like trackers or planners aren’t cures—and they don’t need to be.
They’re helpful when:
- You’re tired of guessing
- You want structure without rigidity
- You need clarity more than motivation
Used gently, they create awareness without pressure.
That shift—from reacting to observing—made all the difference for me.
Final Thoughts
Gut health after 40 isn’t about limitation. It’s about responsiveness.
When you stop assuming your body will adapt automatically and start supporting it intentionally, confidence returns. Not because everything is perfect—but because you’re no longer caught off guard.
If you’re dealing with digestive changes later in life, you’re not behind.
You’re just learning how your body works now.
And that knowledge is power.
If you’re looking for a practical companion to this, I’ve created a free daily gut health tracker.
It’s a simple way to notice patterns in digestion, energy, and stress over time — without changing your diet or routine.
You can find it here: [Gut Health After 40 — Free Daily Tracker]
Optional Resources (Non-Prescriptive)
- The Mind-Gut Connection — Emeran Mayer, MD (Amazon)
- Fiber Fueled — Will Bulsiewicz, MD (Amazon)
- FREE 7-Day Gut Health Tracker
Disclosures
Medical Disclaimer:
This content is for educational purposes only and does not replace professional medical advice.
AI Usage Disclosure:
This article was drafted and refined with the assistance of AI-supported writing tools and reviewed for clarity, accuracy, and authenticity.
Affiliate Disclosure:
Some referenced resources may include affiliate links. As an Amazon Associate, I may earn a small commission at no additional cost to you. “The Gut-Health Productivity Toolkit “ is a link to my Etsy store.













You must be logged in to post a comment.